understanding diagnostic challenges in recognizing celiac disease symptoms effectively
The Complexity of Celiac Disease Symptoms
Celiac disease is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Despite affecting approximately 1% of the global population, it remains significantly underdiagnosed. This is primarily due to the wide variety of symptoms that can manifest, often overlapping with other conditions.
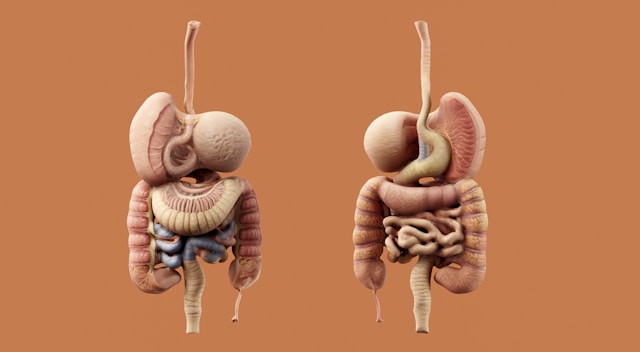
Gastrointestinal Symptoms: More than Just Digestive Issues
The most commonly recognized symptoms of celiac disease are those affecting the gastrointestinal tract. These include chronic diarrhea, constipation, bloating, and abdominal pain. However, not all patients exhibit these symptoms prominently, which complicates diagnosis. For instance, a study conducted by the Mayo Clinic found that only about 60% of individuals with confirmed celiac disease reported diarrhea as a primary symptom.
Non-Gastrointestinal Symptoms: The Hidden Indicators
A significant challenge in diagnosing celiac disease lies in its non-gastrointestinal symptoms. These can include anemia, osteoporosis, fatigue, skin rashes (dermatitis herpetiformis), and neurological issues such as headaches or even depression. Consider this scenario: a patient presenting with anemia and chronic fatigue might be suspected to have iron-deficiency anemia alone, potentially overlooking an underlying celiac condition.
Overlapping Symptoms with Other Disorders
Several conditions share symptoms with celiac disease, further complicating its diagnosis. For example, Irritable Bowel Syndrome (IBS) and lactose intolerance can present with similar digestive disturbances. A patient with IBS may experience alternating constipation and diarrhea, resembling the gastrointestinal distress seen in celiac disease.
Differential Diagnosis: A Critical Step
To differentiate celiac disease from other disorders, a comprehensive differential diagnosis is essential. This often involves:
- Serological Tests: Initial screening tests like tissue transglutaminase antibodies (tTG-IgA) are highly sensitive but not definitive.
- Endoscopic Biopsy: A biopsy of the small intestine remains the gold standard for diagnosis, though invasive.
- Genetic Testing: HLA-DQ2 and HLA-DQ8 testing can rule out celiac disease if negative but cannot confirm it if positive.
These tools help clinicians distinguish celiac disease from disorders such as Crohn's disease or small intestinal bacterial overgrowth (SIBO), which also cause similar malabsorption issues.
The Role of Non-Traditional Presentations
One of the key diagnostic challenges is recognizing non-traditional presentations of celiac disease. Patients might present solely with neurological symptoms like ataxia or peripheral neuropathy without any gastrointestinal signs. In such cases, a high index of suspicion is required from healthcare providers.
Case Example: Silent Celiac Disease
A 42-year-old woman reports to her general practitioner with persistent migraines and fatigue but denies any digestive problems. After several months of treatment for migraine without improvement, her neurologist considers testing for celiac disease due to persistent neurological symptoms. A positive tTG-IgA test leads to a confirmatory biopsy that reveals villous atrophy typical of celiac disease.
Practical Approaches for Clinicians
Given these challenges, clinicians must adopt a comprehensive and systematic approach when assessing potential celiac disease. Here are some practical steps:
- Maintain an Inclusive Differential: Always consider celiac disease in cases of unexplained chronic conditions that do not respond to standard treatments.
- Holistic Patient History: A thorough patient history including family medical history, diet analysis, and symptom chronology can provide crucial diagnostic clues.
- Multi-Disciplinary Collaboration: Work closely with dietitians, gastroenterologists, and neurologists when evaluating complex cases.
The Impact of Delayed Diagnosis
Failure to promptly diagnose celiac disease can lead to long-term health complications such as increased risk for certain cancers and osteoporosis. It's crucial to understand that effective management begins with accurate diagnosis followed by strict adherence to a gluten-free diet.
Education and Awareness: Crucial Components
The ongoing education of both healthcare providers and the public about the diverse manifestations of celiac disease is critical. Enhanced awareness can lead to earlier detection and improve patient outcomes significantly.
Conclusion: Navigating Diagnostic Challenges
Celiac disease remains a complex disorder with varied symptoms that can masquerade as numerous other conditions. Recognizing its diverse presentations requires vigilance and a multi-faceted approach by healthcare professionals. Continued research and education are vital in improving diagnostic strategies and ultimately enhancing the quality of life for those affected by this autoimmune condition.






