The Role of Gene Editing in Custom Cancer Treatments for Patients
Revolutionizing Cancer Treatment with CRISPR Technology
In recent years, the field of oncology has witnessed a paradigm shift with the introduction of gene editing technologies, particularly CRISPR-Cas9. This innovative tool offers unprecedented opportunities for customizing cancer treatments to individual patients' needs. With the ability to precisely modify genetic sequences, CRISPR holds the promise of transforming personalized medicine into a practical reality.
One of the most compelling applications of CRISPR is its use in custom cancer treatments. By targeting specific mutations in a patient's tumor cells, scientists can develop more effective and tailored therapies. This article explores how CRISPR technology is being utilized in groundbreaking clinical trials, focusing on a recent case study involving a patient with advanced melanoma.
The Mechanism of CRISPR in Cancer Therapy
CRISPR, short for Clustered Regularly Interspaced Short Palindromic Repeats, is a genome-editing tool that allows researchers to make precise changes to DNA sequences. It consists of two key components: the Cas9 enzyme, which acts like a pair of molecular scissors, and a guide RNA (gRNA) that directs Cas9 to the specific location in the genome that needs editing.
In the context of cancer therapy, CRISPR can be used to knock out oncogenes—genes that have the potential to cause cancer—or repair tumor suppressor genes that are malfunctioning. This targeted approach aims to halt the proliferation of cancer cells while sparing healthy tissue, thereby reducing side effects and improving patient outcomes.
A Groundbreaking Clinical Trial: Personalized Treatment for Melanoma
Recently, a clinical trial led by a consortium of international researchers successfully demonstrated the potential of CRISPR in treating advanced melanoma. The trial focused on a 57-year-old patient who had exhausted conventional treatment options and showed no response to chemotherapy or immunotherapy.
Patient Selection and Genetic Profiling
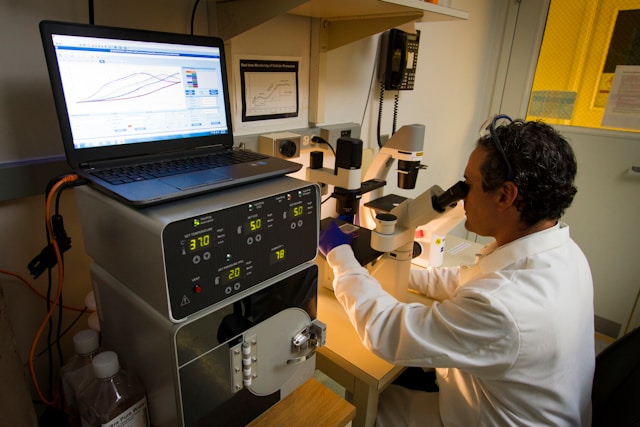
The first step in the trial was comprehensive genetic profiling of the patient's tumor. Researchers used next-generation sequencing (NGS) to identify specific genetic mutations driving the patient's melanoma. This data was crucial in designing a customized CRISPR intervention strategy.
The patient's tumor exhibited several known mutations in genes such as BRAF and NRAS, which are common targets in melanoma but had not responded to existing targeted therapies. The researchers aimed to edit these mutations directly using CRISPR.
Designing and Delivering CRISPR Treatment
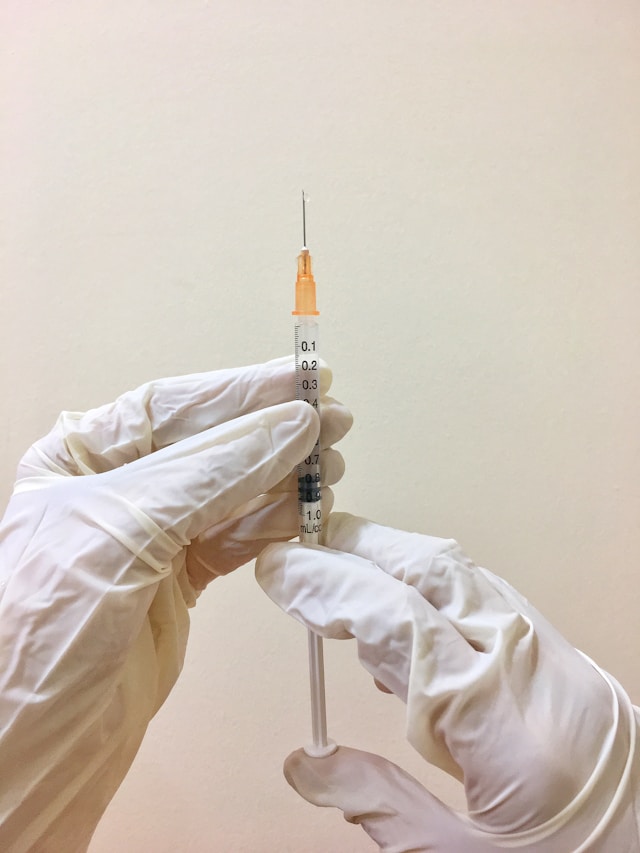
The next stage involved designing guide RNAs specific to the identified mutations. These gRNAs were paired with the Cas9 enzyme and delivered into the patient's tumor cells using lipid nanoparticles, a method that ensures efficient uptake and minimal off-target effects.
Upon delivery, the CRISPR-Cas9 system successfully edited the DNA at target sites, correcting faulty sequences or disabling oncogenic pathways. This intervention was meticulously monitored through frequent biopsies and advanced imaging techniques.
Results: Tumor Reduction and Patient Outcomes
The results of this trial were nothing short of remarkable. Within three months of CRISPR treatment, imaging studies revealed a significant reduction in tumor size—by approximately 60%—and stabilized disease progression. Moreover, the patient reported an improved quality of life with minimal side effects.
This case underscores the potential of CRISPR not just as a therapeutic tool but also as a beacon of hope for patients with limited options. The precision of gene editing enables interventions that are tailored to each patient's unique genetic landscape.
Challenges and Ethical Considerations
Despite its promise, the application of CRISPR in cancer therapy is not without challenges. One major concern is off-target effects—unintended genetic modifications that could lead to adverse outcomes. Ongoing research aims to enhance CRISPR specificity through advances in gRNA design and delivery mechanisms.
Ethical considerations also play a significant role in gene editing, especially concerning germline modifications that could affect future generations. However, current cancer therapies focus on somatic cells, which do not pose these hereditary risks.
The Future of Personalized Medicine
CRISPR's role in custom cancer treatments exemplifies the broader trend towards precision medicine. As our understanding of genetic underpinnings grows, we can anticipate more tailored therapeutic approaches across various cancers.
- Research Collaboration: Continued collaboration among researchers worldwide will accelerate advancements in CRISPR technology and its applications in oncology.
- Regulatory Frameworks: Developing comprehensive regulatory frameworks will ensure safe and ethical implementation of gene editing therapies.
- Integration with AI: Leveraging artificial intelligence can enhance data analysis from genetic profiling, facilitating quicker identification of actionable mutations.
Conclusion
As this case study illustrates, gene editing holds transformative potential for cancer treatment. Through continued research and innovation, we can look forward to a future where personalized medicine becomes standard practice, offering hope and healing to patients once deemed untreatable.