The Future of Severe Asthma Treatment: Promising Biologic Options
The Rise of Biologics in Asthma Management
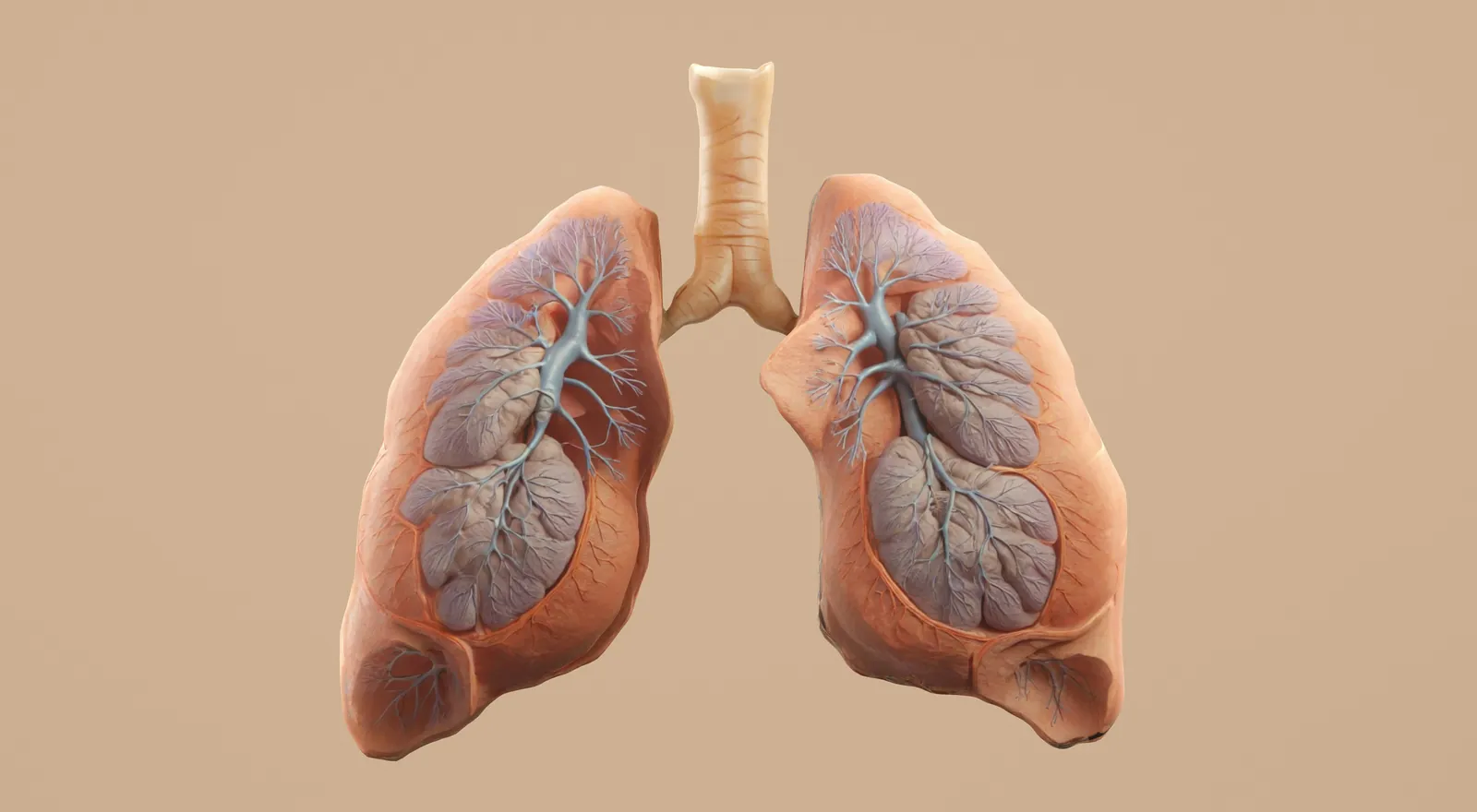
Severe asthma, a subset affecting a smaller but significant group of asthma sufferers, often resists conventional treatments like inhaled corticosteroids and bronchodilators. In recent years, biologic medications have emerged as a transformative option for managing this persistent condition. These targeted therapies offer hope by addressing the underlying biological pathways contributing to inflammation and airway hyper-responsiveness.
Biologics are complex molecules engineered to target specific components of the immune system. Unlike traditional asthma therapies that provide symptomatic relief, biologics intervene at the molecular level to prevent inflammation and reduce exacerbations.
Understanding Biologic Mechanisms
Targeting Interleukins
Interleukins are cytokines that play a crucial role in orchestrating immune responses. Several biologics have been developed to inhibit interleukins involved in asthma's inflammatory cascade:
- IL-5 Inhibitors: Medications like mepolizumab and reslizumab target interleukin-5, a cytokine responsible for eosinophil activation and survival. By reducing eosinophil levels, these drugs decrease airway inflammation.
- IL-4/IL-13 Dual Inhibitors: Dupilumab works by inhibiting the IL-4 receptor alpha subunit, which blocks both IL-4 and IL-13 signaling pathways. This action reduces inflammation and mucus production.
IgE Antagonists
Omalizumab, an anti-IgE antibody, was one of the first biologics approved for asthma. It binds to immunoglobulin E (IgE), preventing it from interacting with mast cells and basophils, thus reducing allergic inflammation.
Evaluating Effectiveness and Patient Eligibility
Biologics are not suitable for every patient with asthma. They are typically reserved for individuals with severe asthma who exhibit specific phenotypes or biomarkers:
Eosinophilic Asthma
Patients with elevated eosinophil counts are ideal candidates for IL-5 inhibitors. A blood test measuring eosinophils can help determine eligibility.
Allergic Asthma
Those with elevated serum IgE levels may benefit from omalizumab. A skin prick test or a specific IgE blood test can aid in identifying eligible patients.
In all cases, the decision to start biologic therapy should be based on a comprehensive assessment by a specialist, often requiring collaboration between allergists, pulmonologists, and primary care physicians.
Pros and Cons of Biologic Therapy
The introduction of biologics has revolutionized severe asthma treatment, but they come with their own set of advantages and disadvantages:
Pros
- Targeted Action: Biologics provide precise interventions by targeting specific immune pathways, which minimizes systemic side effects.
- Reduction in Exacerbations: Clinical trials have shown that biologics significantly decrease the frequency of severe asthma attacks.
- Improved Quality of Life: Patients report better symptom control and overall life quality improvements.
Cons
- Cost: Biologics are expensive, which can limit accessibility and affordability.
- Administration: Most biologics require injections, which might be cumbersome for some patients.
- Variable Response: Not all patients respond equally; some may see little to no benefit despite meeting eligibility criteria.
A Framework for Monitoring Treatment Outcomes
An effective framework for monitoring outcomes in patients receiving biologics includes several components:
Regular Follow-Ups
Schedulem regular visits to assess symptoms, lung function tests, and quality of life questionnaires. This helps in tracking progress and identifying any necessary treatment adjustments.
Biomarker Monitoring
Routine blood tests for eosinophils or IgE can help gauge treatment effectiveness and guide potential dosage modifications.
Patient Education
Educate patients on the importance of adherence, potential side effects, and when to seek medical attention. Ensuring patients understand their treatment can enhance engagement and outcomes.
The Future Outlook for Biologic Therapies
The future of severe asthma treatment is promising with continuous advancements in biologic therapies. Research is ongoing to identify additional targets within the inflammatory cascade and develop next-generation biologics with even greater precision and fewer side effects. There is also a push toward developing oral formulations that could simplify administration and increase patient compliance.
As our understanding of asthma phenotypes deepens, personalized medicine will likely become a cornerstone of severe asthma management. This approach will enable clinicians to tailor treatments based on individual biological markers, optimizing efficacy while minimizing unnecessary interventions.
The integration of artificial intelligence into treatment protocols might further enhance personalized care by predicting patient response to biologics based on complex data analysis. Such advancements underscore a hopeful future where severe asthma may become a manageable condition with minimal impact on patients' lives.