How Customized Meal Plans Help in Preventing Major Health Issues

The Power of Personalized Nutrition
In today's fast-paced world, where dietary habits significantly influence our overall health, the concept of personalized nutrition is gaining momentum. Customized meal plans are not just about counting calories; they're crafted to meet individual needs and preferences, taking into account medical history, lifestyle, and genetic predispositions. This tailored approach can be pivotal in preventing major health issues such as diabetes and heart disease.
Personalized meal plans harness the power of nutrition to promote wellness and prevent chronic conditions. By considering an individual's unique biochemistry, personalized diets can help modulate inflammatory responses, improve metabolic health, and support heart function. But how exactly do these meal plans work, and what are their benefits compared to traditional dietary guidelines?
Traditional Diets vs. Customized Meal Plans
Traditional Diets: One Size Fits All
For decades, dietary guidelines have often promoted a 'one-size-fits-all' approach. These generic plans typically focus on broad recommendations such as reducing fat intake or increasing fiber consumption. While these guidelines have merit, they fail to address the complexities of individual nutritional needs.
- Pros: Simplicity and ease of understanding for the general public.
- Cons: Lack of personalization can result in suboptimal outcomes for those with specific health issues or dietary restrictions.
Customized Meal Plans: Tailored to You
Customized meal plans take personalization to the next level by integrating personal health data to tailor dietary advice. These plans can be created with input from dietitians and nutritionists who consider factors like allergies, food intolerances, metabolic conditions, and even genetic information.
- Pros: Highly individualized and potentially more effective in preventing and managing chronic diseases.
- Cons: Can be more time-consuming and may require professional guidance.
The Role of Genetics in Personalized Nutrition
The field of nutrigenomics explores the relationship between our genes, nutrition, and health outcomes. Genetic testing can reveal specific markers that indicate susceptibility to conditions such as obesity, type 2 diabetes, or cardiovascular disease. With this information, a customized meal plan can be devised to mitigate these risks.
For instance, individuals with a genetic predisposition for high cholesterol might benefit from a diet rich in omega-3 fatty acids found in fish and flaxseeds. Conversely, someone with lactose intolerance would require adjustments that ensure adequate calcium intake from non-dairy sources.
Impact on Chronic Disease Prevention
Diabetes Management
Customized meal plans play a crucial role in managing blood sugar levels for individuals at risk of or living with diabetes. By focusing on low-glycemic-index foods, balanced macronutrients, and portion control, these plans can prevent blood sugar spikes and insulin resistance.
An example could involve incorporating more whole grains like quinoa and barley, which release glucose slowly into the bloodstream, thereby reducing the risk of developing type 2 diabetes.
Heart Health Optimization
Heart disease remains a leading cause of mortality worldwide. Personalized nutrition can effectively manage risk factors such as high blood pressure, elevated cholesterol levels, and obesity. By emphasizing foods rich in antioxidants and healthy fats, these meal plans can improve cardiovascular outcomes.
A person with a family history of heart disease might be advised to increase their intake of heart-friendly foods such as avocados, nuts, and leafy greens while reducing salt and saturated fat consumption.
Practical Steps for Creating a Personalized Meal Plan
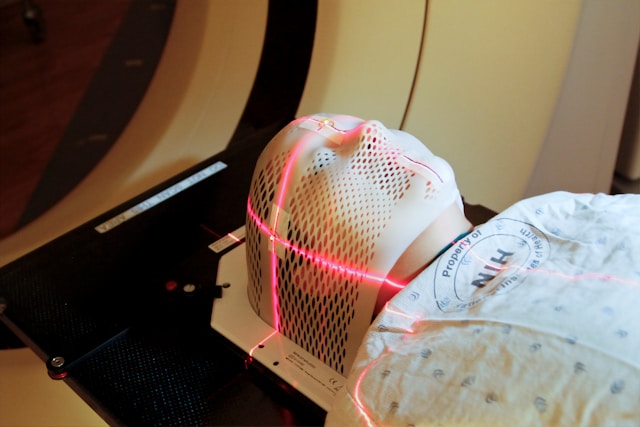
- Health Assessment: Begin with a comprehensive evaluation of current health status, including lab tests for blood sugar levels, cholesterol profiles, and any existing medical conditions.
- Set Specific Goals: Identify clear health goals such as weight management, blood sugar stabilization, or cholesterol reduction.
- Dietary Preferences and Restrictions: Take into account food allergies, intolerances, cultural preferences, and ethical considerations (e.g., vegetarianism).
- Nutritional Consultation: Work with a registered dietitian to interpret health data and develop a structured plan.
- Monitor and Adjust: Regular follow-ups to track progress and make necessary dietary adjustments.
The Future of Personalized Nutrition
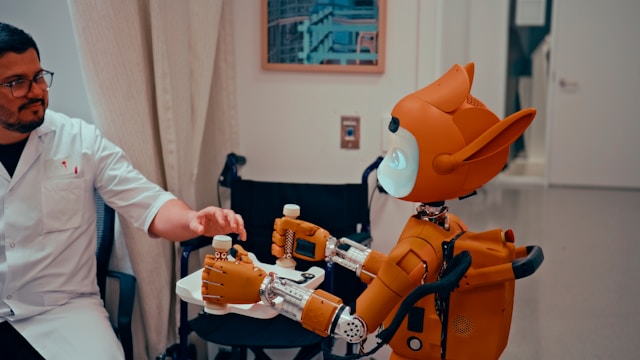
The future of preventive healthcare is likely to see an integration of technology with personalized nutrition. Wearable devices that monitor dietary intake and physiological responses could offer real-time data, allowing for even more precise tailoring of meal plans. Artificial intelligence may also play a role by analyzing vast datasets to provide predictive insights into how certain foods affect individual health outcomes.
As research continues to unravel the complexities of human metabolism and its interaction with diet, the scope for preventing chronic diseases through customized nutrition will only broaden. This shift towards personalization promises a future where preventive care is not just reactive but proactive and anticipatory.
Conclusion
The impact of customized meal plans on preventing major health issues is profound. By acknowledging the uniqueness of each individual and leveraging personal health data, personalized nutrition offers a powerful tool in the fight against chronic diseases such as diabetes and heart disease. As we embrace this tailored approach to eating, we move closer to a future where preventive care is optimized for each individual's journey to optimal health.