guidelines for preparing and giving biologic injections for RA
Understanding Biologic Treatments for Rheumatoid Arthritis
Biologic treatments have revolutionized the management of rheumatoid arthritis (RA), offering targeted approaches that can significantly alleviate symptoms and improve quality of life. These advanced medications, derived from living cells, help modify the immune response that drives inflammation in RA. Common biologics include Tumor Necrosis Factor (TNF) inhibitors, Interleukin-6 (IL-6) inhibitors, and B-cell inhibitors, among others.
Due to their complexity, biologics are typically administered via injections or infusions. This article focuses on providing healthcare professionals and patients with a comprehensive checklist for administering biologic injections safely and effectively.
Pre-Administration Patient Assessments
Reviewing Patient History
Before initiating biologic treatment, it’s crucial to conduct a thorough patient history review. Consider factors such as:
- Previous medication responses: Document past therapies and any adverse reactions.
- Current health status: Assess for infections, as biologics can suppress the immune system.
- Vaccination history: Ensure vaccinations are up-to-date, especially live vaccines which may be contraindicated during biologic therapy.
Baseline Laboratory Testing
Prior to the first injection, obtain baseline laboratory tests to monitor the patient’s overall health and detect any potential contraindications. Recommended tests may include:
- CBC (Complete Blood Count): To evaluate bone marrow function.
- Liver function tests: As many biologics are metabolized in the liver.
- TB test (Tuberculin Skin Test or IGRA): To rule out latent tuberculosis, which can be reactivated by biologics.
Preparation of Biologic Injections
Understanding the Medication
Each biologic has unique storage and preparation requirements. It is essential to:
- Read the manufacturer’s instructions: Confirm specific storage temperatures and expiration dates.
- Inspect the medication: Check for discoloration or particulates before use.
Injection Equipment Checklist
Ensure all necessary equipment is ready:
- Sterile needles and syringes (if not using pre-filled syringes)
- Alcohol swabs for disinfecting the injection site
- A sharps disposal container for used needles and syringes
Preparing the Injection Site
Select an appropriate injection site based on the type of injection:
- Subcutaneous injections: Common sites include the abdomen, thigh, or back of the arm.
Cleanse the area with an alcohol swab and allow it to dry completely to reduce infection risk.
Administering the Injection
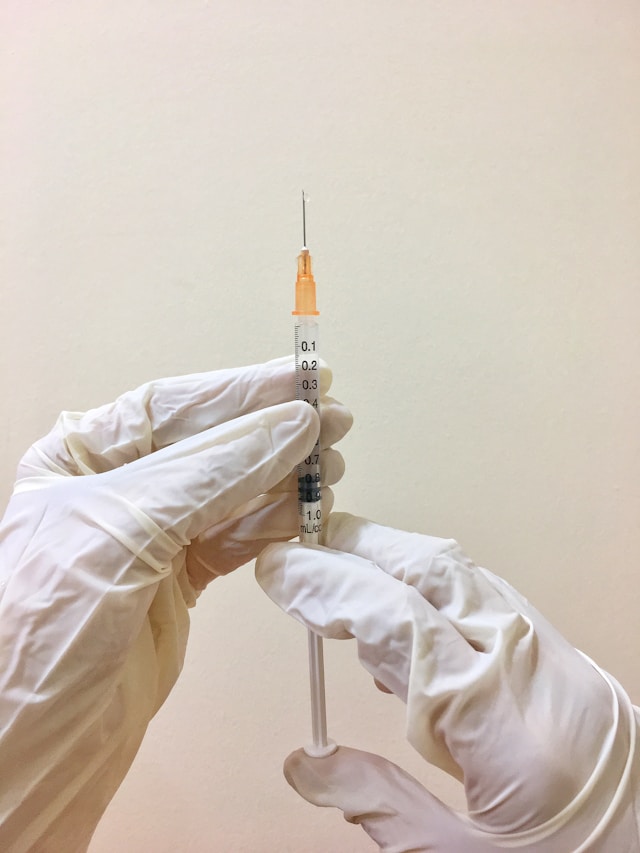
Injection Technique
The following steps outline a typical subcutaneous injection technique:
- Wash hands thoroughly with soap and water.
- Prepare the syringe as instructed by drawing up the correct dose if not using a pre-filled syringe.
- Pinch the skin at the chosen site to create a firm surface.
- Insert the needle at a 45-degree angle for subcutaneous injections.
- Smoothly inject the medication at a steady pace.
- Withdraw the needle and dispose of it immediately in a sharps container.
Troubleshooting Common Issues
If resistance is encountered during injection or discomfort occurs, pause and reassess your technique. Ensure proper angle and needle depth are maintained throughout administration.
Post-Injection Monitoring and Follow-Up
Monitoring for Side Effects
Biologic medications can cause side effects ranging from mild injection site reactions to more severe systemic effects. Common side effects include:
- Redness or swelling at the injection site
- Mild fever or fatigue shortly after administration
Educate patients about these potential reactions and advise them on when to seek medical attention.
Routine Follow-Up Appointments
Regular follow-up visits are essential to monitor treatment effectiveness and adjust dosing as needed. During these visits:
- Evaluate symptom improvement using standardized assessment tools like the DAS28 (Disease Activity Score).
- Check laboratory values periodically to ensure no adverse changes occur due to treatment.
Conclusion
The administration of biologic injections for rheumatoid arthritis requires meticulous preparation and attention to detail. By following these guidelines, healthcare providers can ensure that these powerful medications are delivered safely and effectively, maximizing their therapeutic potential while minimizing risks. Patients should feel empowered through education and ongoing support, fostering a collaborative approach to managing their RA effectively.