Examining Persistent Pain and Exhaustion in Chronic Lyme Disease

Understanding Chronic Lyme Disease
Chronic Lyme disease, often referred to as Post-Treatment Lyme Disease Syndrome (PTLDS), presents a complex set of symptoms that can significantly impact an individual's quality of life. While it stems from the initial infection with the Borrelia burgdorferi bacteria, its chronic form continues to puzzle researchers and healthcare providers. Patients often report a range of persistent symptoms long after standard treatment courses.
The Challenge of Diagnosis
One of the major challenges with chronic Lyme disease is its diagnosis. Symptoms such as persistent fatigue and musculoskeletal pain often overlap with those of other conditions like fibromyalgia and chronic fatigue syndrome, making it difficult to pinpoint Lyme as the cause. Furthermore, standard blood tests may not always provide conclusive results for chronic cases, leading to frustration and uncertainty for both patients and practitioners.
A practical approach for clinicians involves comprehensive patient history taking, focusing on previous tick exposure, symptom progression, and ruling out other potential causes through differential diagnosis. Collaboration with specialists such as rheumatologists or infectious disease experts can provide additional insights and guidance.
Exploring Persistent Symptoms
Fatigue: A Debilitating Symptom
Fatigue associated with chronic Lyme disease is more than just feeling tired. It can be overwhelming and debilitating, affecting daily activities and overall well-being. Patients describe it as a profound lack of energy that doesn't improve with rest, impacting both physical and mental capacities.
Example Scenario: Jane, a 45-year-old teacher, finds herself struggling to maintain her usual workload. Despite adequate sleep, she wakes up exhausted and relies heavily on caffeine just to get through the morning. Her once active lifestyle has diminished due to the persistent fatigue she cannot seem to shake.
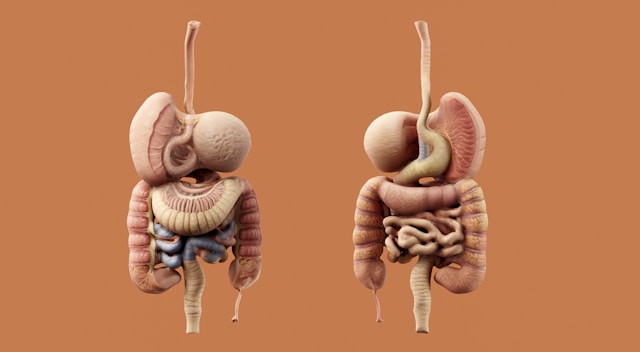
Musculoskeletal Pain: Beyond Aches
The musculoskeletal pain associated with chronic Lyme disease often manifests as joint pain, muscle aches, and sometimes neurological discomfort like tingling sensations. Unlike typical post-exercise soreness, this pain can be chronic and unpredictable, severely impacting mobility and daily function.
A useful strategy for managing this pain involves a combination of medication management, physical therapy, and lifestyle adjustments. Patients might work closely with pain specialists to create personalized plans that could include anti-inflammatory drugs or low-impact exercise routines.
Overlapping Symptoms with Other Conditions
As mentioned, chronic Lyme disease shares several symptoms with conditions such as fibromyalgia, chronic fatigue syndrome, and autoimmune diseases. This overlap complicates diagnosis and management but understanding these connections can aid in creating more effective treatment plans.
- Fibromyalgia: Both conditions share symptoms of widespread musculoskeletal pain, fatigue, and cognitive difficulties. However, fibromyalgia is generally diagnosed based on specific tender points and symptom duration.
- Chronic Fatigue Syndrome (CFS): CFS is characterized by extreme fatigue lasting more than six months, which doesn't improve with rest. Like chronic Lyme disease, CFS has no definitive diagnostic test but is identified through symptom assessment and exclusion of other causes.
Effective Management Strategies
Multidisciplinary Approach
Treating chronic Lyme disease effectively requires a multidisciplinary approach that addresses both the physical and psychological aspects of the condition. This often involves a team of healthcare professionals including primary care physicians, specialists, mental health professionals, and physical therapists.
Collaborative care plans might include:
- Pharmacological Interventions: Use of antibiotics if necessary for ongoing bacterial presence, alongside pain management medications such as NSAIDs or neuropathic agents.
- Cognitive Behavioral Therapy (CBT): CBT can help patients develop coping strategies for dealing with chronic symptoms and improve mental health outcomes.
- Nutritional Support: Dietitians can assist in crafting anti-inflammatory diets that support immune function and overall health.
Patient Empowerment
Empowering patients is crucial in managing chronic Lyme disease. Education about the condition, realistic goal setting, and self-management skills are key components. Encouraging patients to track their symptoms using journals or digital apps can facilitate better communication with healthcare providers and enable more tailored treatment adjustments.
Practical Tips for Managing Daily Life
Navigating life with chronic Lyme disease requires adaptability and practical strategies to manage daily challenges effectively:
- Pacing Activities: Encourage breaking tasks into manageable chunks and resting before fatigue sets in.
- Prioritizing Tasks: Focus on completing essential activities during periods of higher energy.
- Seeking Support: Engaging with support groups or online communities can provide emotional support and shared experiences.
Ultimately, while chronic Lyme disease poses significant challenges due to its persistent symptoms like fatigue and musculoskeletal pain, a comprehensive approach involving accurate diagnosis, multifaceted treatment strategies, and patient empowerment can lead to improved management and enhanced quality of life.