Evaluating How Effective Preventive Screenings Can Be for Heart Health Management
The Importance of Preventive Screenings in Heart Health
Heart disease remains the leading cause of death worldwide. This stark reality underscores the vital role that preventive screenings play in managing heart health. By identifying risk factors and early signs of cardiovascular issues, these screenings can significantly alter the trajectory of an individual's health outcomes.
Current statistics from the American Heart Association indicate that over 80% of cardiovascular diseases can be prevented through early intervention and lifestyle changes, many of which are prompted by findings during routine screenings.
Understanding the Benefits of Early Detection
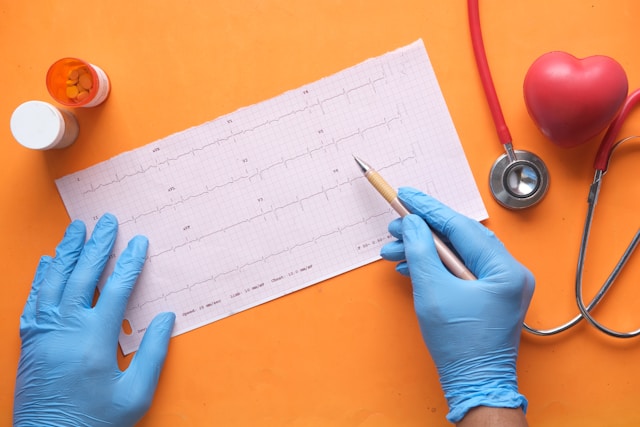
The primary benefit of preventive screenings is their ability to detect conditions such as hypertension, high cholesterol, and early atherosclerosis before they progress to more serious stages. Detecting these conditions early can lead to prompt lifestyle modifications and medical interventions that may prevent heart attacks or strokes.
- Hypertension Screening: Regular blood pressure checks can help diagnose hypertension early, allowing patients to manage it through lifestyle changes and medication.
- Cholesterol Levels: Lipid panels provide insight into cholesterol levels, indicating whether dietary adjustments or medications like statins are necessary.
- Diabetes Screening: Since diabetes significantly increases cardiovascular risk, early detection through glucose tests can prompt necessary lifestyle changes or treatment plans.
Concrete Example: Early Hypertension Detection
Consider a 55-year-old patient, James, who attends an annual health checkup. A routine screening reveals his blood pressure is 150/95 mmHg, classified as stage 1 hypertension. The physician recommends lifestyle changes including a low-sodium diet, regular exercise, and stress management techniques. Within six months, James’s blood pressure normalizes, averting potential cardiovascular events.
The Risk of Over-diagnosis and Its Implications
Despite their benefits, preventive screenings are not without their trade-offs. Over-diagnosis is a significant concern, where non-threatening abnormalities are identified as serious conditions, leading to unnecessary anxiety and treatment.
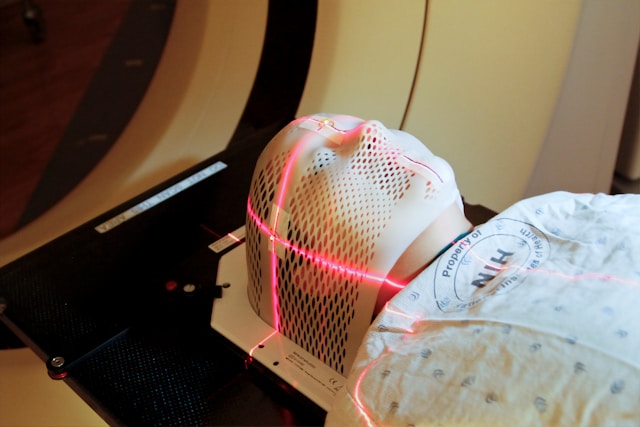
For example, coronary artery calcium (CAC) scoring can sometimes identify calcium build-up that isn't clinically significant but prompts invasive procedures. It's crucial for healthcare providers to balance thoroughness with prudence to avoid undue stress and interventions for patients.
Clinical Workflow for Balancing Screening Outcomes
- Initial Screening: Conduct baseline assessments like lipid panels and blood pressure measurements.
- Risk Assessment: Evaluate individual risk factors such as age, family history, and lifestyle.
- Consultation: Discuss findings with patients, emphasizing the difference between modifiable risk factors and genetic predispositions.
- Shared Decision-Making: Engage patients in deciding the next steps, considering both the potential benefits and risks of further testing.
Best Practices for Patient Decision-Making in Preventive Care
Successful preventive care hinges on effective patient engagement and education. By fostering an understanding of the pros and cons of different screening tests, patients can make informed decisions about their health management strategies.
Scenario: Shared Decision-Making in Action
Susan, a 60-year-old with a family history of heart disease, discusses her screening results with her physician. They find elevated LDL cholesterol levels. The physician explains the benefits and drawbacks of starting statin therapy versus attempting lifestyle changes first. Together, they decide on a three-month trial period focusing on diet and exercise before reconsidering medication.
Checklist for Patient Engagement
- Education: Provide clear information about each test’s purpose and potential outcomes.
- Communication: Encourage open discussions about fears or misconceptions regarding screenings.
- Options: Outline alternative monitoring strategies if patients are hesitant about certain tests.
- Follow-up: Schedule regular check-ins to discuss progress and reassess decisions.
Conclusion: Striking a Balance
The effectiveness of preventive screenings in heart health management lies in their capacity to provide early warnings without causing unnecessary alarm or treatment. By employing balanced approaches tailored to individual needs, healthcare providers can optimize patient outcomes while minimizing risks associated with over-diagnosis.
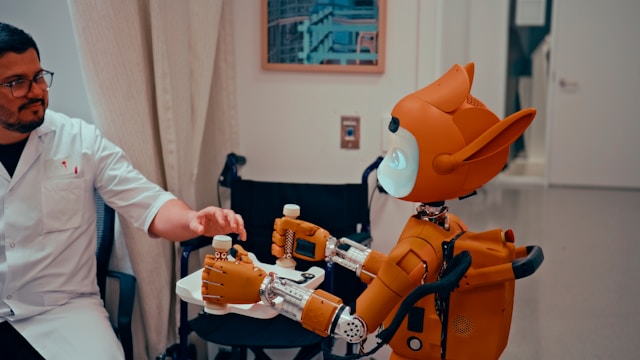
The future of heart health management is promising as technological advancements continue to refine screening methods, making them less invasive yet more informative. Emphasizing personalized care strategies will ensure that screenings remain a cornerstone in preventive medicine without compromising patient well-being.