Assessing Long-term Health Outcomes Using Genetic Screening Methods

The Role of Genetic Screening in Preventive Care
In the evolving landscape of healthcare, genetic screening has emerged as a powerful tool in preventive care. By identifying individuals at risk for hereditary conditions, genetic testing facilitates early interventions and personalized health strategies, potentially transforming how we approach healthcare on both individual and systemic levels.
Understanding Genetic Screening
Genetic screening involves analyzing DNA to identify changes or variants that may indicate a higher risk of developing certain health conditions. This process can be utilized to assess predispositions to various diseases such as cancers, cardiovascular conditions, and genetic disorders like cystic fibrosis or sickle cell anemia.
Methods of Genetic Screening
Common methods of genetic screening include:
- Whole Genome Sequencing: Provides a comprehensive analysis by mapping an individual's entire genetic makeup.
- Targeted Gene Panels: Focus on specific genes known to influence the risk of certain conditions.
- SNP Genotyping: Examines single nucleotide polymorphisms, which are the most common type of genetic variation among people.
These methods offer varying degrees of detail and are selected based on specific clinical needs and patient histories.
Applications in Preventive Care
Genetic screening plays a pivotal role in preventive care by enabling proactive health management. For instance, if a woman carries BRCA1 or BRCA2 gene mutations, which significantly increase her risk of breast and ovarian cancer, she can opt for more frequent screenings or preventive surgeries. Similarly, individuals with a family history of heart disease might benefit from lifestyle changes informed by their genetic risk profile.
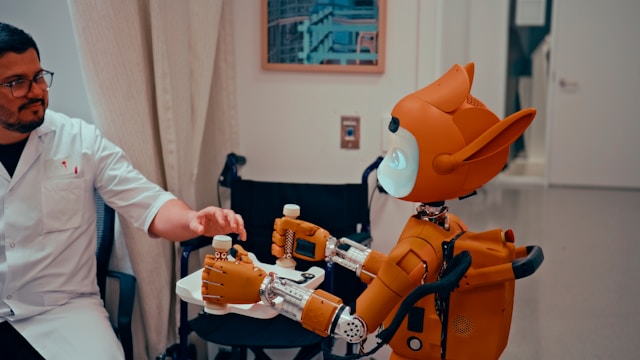
Implementing Targeted Interventions
Armed with insights from genetic tests, healthcare providers can design interventions tailored to individual risk factors. Such strategies might include:
- Lifestyle Modifications: Diet, exercise, and stress management plans tailored to reduce specific risks.
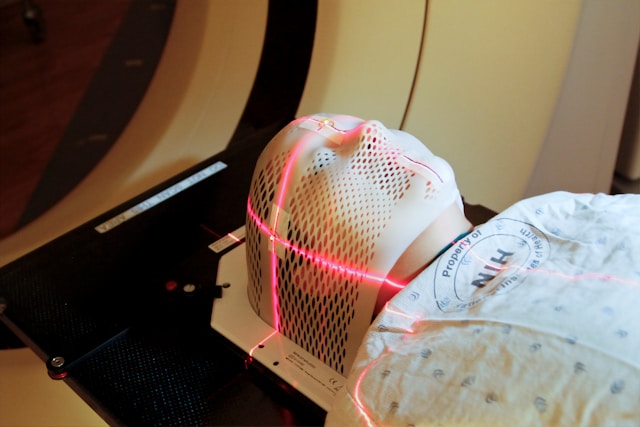
- Surveillance Programs: More frequent monitoring for early detection of potential health issues.
- Prophylactic Treatments: Medications or surgeries to prevent the onset of diseases.
Ethical Implications of Genetic Screening
While genetic screening offers tremendous benefits, it also raises several ethical concerns. Key issues include:
- Privacy and Confidentiality: Ensuring that genetic data is securely stored and shared only with consent.
- Discrimination Risks: The potential for genetic information to be used unfairly in employment or insurance settings.
- Psychological Impact: The anxiety or stress related to learning about one's genetic risks.
Addressing Ethical Challenges
To address these concerns, robust regulatory frameworks are necessary. These might include strict data protection laws, guidelines for ethical use of genetic information, and comprehensive counseling for individuals undergoing testing.
Cost-Effectiveness of Genetic Screening
The economic viability of widespread genetic screening is a topic of significant debate. While initial costs may be high, proponents argue that early detection and intervention can lead to reduced long-term healthcare costs by preventing severe health conditions and avoiding expensive treatments later in life.
Evaluating Economic Benefits
A framework to assess the cost-effectiveness of genetic screening should consider:
- The initial costs of testing and infrastructure development.
- The potential savings from avoided treatments and hospitalizations.
- The broader economic impacts, such as increased productivity and quality of life for individuals who remain healthy longer.
Practical Tips for Implementing Genetic Screening Programs
Healthcare providers looking to integrate genetic screening into preventive care strategies can follow these practical steps:
- Establish Clear Objectives: Define what you aim to achieve with the screening program, whether it's reducing specific disease rates or enhancing overall patient wellness.
- Select Appropriate Technologies: Choose genetic testing methods that align with your objectives and resources.
- Engage Stakeholders: Involve patients, healthcare professionals, policymakers, and community leaders in planning and implementation.
- Ensure Adequate Training: Equip healthcare staff with the necessary knowledge to interpret results and counsel patients effectively.
- Monitor and Evaluate Outcomes: Regularly assess the program's impact on health outcomes and make adjustments as needed.
A Mini-Framework for Personalized Health Strategies
This mini-framework outlines a step-by-step process for leveraging genetic screening to develop personalized health strategies:
- Risk Assessment: Conduct comprehensive genetic screenings to identify potential risks.
- Create Risk Profiles: Develop individual risk profiles that incorporate genetic data alongside traditional risk factors like age and lifestyle.
- Design Interventions: Tailor preventive measures—such as lifestyle modifications, regular screenings, or medications—to address identified risks.
- Patient Education: Inform patients about their genetic risks and involve them actively in managing their health through informed decision-making.
- Continuous Monitoring: Use ongoing assessments to track patient progress and refine strategies over time.
This framework enables healthcare providers to not only predict but also effectively manage health outcomes through personalized care plans based on genetic information.